It has long been recognised that the size of a subject's lungs is related to their physical size. Standing height has been used as an imperfect measure of size in relation to lung function when trying to predict a subject's lung function. It has been noted that men and women of the same age and height have different lung function because the relationship between height and lung size differs between the sexes [1]. Hence there have been separate lung function reference equations for men and women.
It has also been noted that people of African ancestry have a different relationship between standing height and lung function compared to people of European ancestry [2]. This led to separate equations being derived for peoples of different ancestry [3]. The reason behind this ancestry related difference in the relationship between standing height and lung function is of considerable interest. It has been suggested this may be due to poorer socio-economic status (SES) throughout life in people of African ancestry when compared to Europeans and poorer SES has been shown to lead to lower lung function [4].
It is thought that Homo Sapiens originated in Africa more than 250,000 years ago. People then migrated in search of more suitable living conditions and evolution favoured certain characteristics in relation to where people lived. Species adapted to living near the equator have longer limbs and thinner bodies to facilitate heat loss. Whereas species adapted to living near the poles or in the cold at altitude have shorter limbs/appendages and rounder bodies to minimise surface area in order to preserve heat. This is called Allen's law [5] which pertains to all homeothermic species.
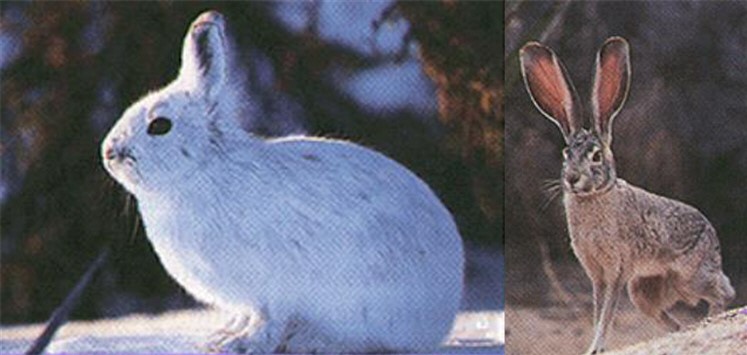
Pictures of an arctic hare on the left with short ears and limbs versus a desert hare on the right with long ears and limbs illustrates this point.
In humans the Inuit, who are indigenous to the Arctic and Subarctic regions of North America, have rounder bodies and shorter limbs than say Europeans and Ethiopians to facilitate heat retention. People adapted to living near the equator in Africa such as Kenyans and Ethiopians have longer legs and arms in relation to their height than Europeans to facilitate heat loss. These adaptations affect the relationship between standing height and estimates of thoracic size and hence lung function. It is important to note that peoples now living near the equator in the Americas, such as Panama, have in recent times largely migrated south from North America.
When applying lung function prediction equations derived from European subjects to the Inuit their lung function appears supranormal [6,7,8], despite them having a much lower SES than Canadians of European ancestry [9]. The apparently supranormal lung function for the Inuit seen when using prediction equations for Europeans can be completely remedied by taking into account their shorter leg length [6]. Conversely applying equations derived from European subjects to people of African descent makes their lung function appear to be low. Studies that have tried to differentiate the magnitude of the effect of anthropometric differences and of SES differences on lung function have found that 35% of the differences in lung function were due to anthropometric differences but only 7% could be accounted for by the effect of lower SES [10,11,12].
Attention has been drawn to the possibility of racism with regard to how lung function test results are used and that this might lead to missed diagnoses [13]. In 2023 the Global Lung Initiative group published a new set of spirometry reference equations that were proposed to be applicable globally with no account being taken of a subject's ancestry [14]. The equations were derived from a weighted average for all the individual data that were available to them at the time and were promoted as being 'race neutral'. The recent ATS workshop on Ancestry and Lung Function recommended using these 'race neutral' equations as a way to avoid possible racism in medical practice [15].
Racism in medical practice would occur if a patient had an adverse or prejudicial outcome on the basis of their ancestry. This could arise if accounting for a person's ancestry led to a prejudicial outcome. However, racism would also arise if a clinician failed to take into account a person's ancestry and this omission led to a prejudicial outcome. In the context of lung function prediction this means that we need to know if when assessing a patient's lung function is the patient's clinical management or outcome prejudiced by either ignoring or taking into account their ancestry.
The combined population samples from NHANES 2007/8, 2009/10 and 2010/12 comprised 2874 non-Hispanic White men and 1147 non-Hispanic Black men (ratio 2:1), and 2825 non-Hispanic White women and 1467 non-Hispanic Black women (ratio 2:1) aged at least 20. To look at the effect of using ancestry specific versus ancestry neutral equations the key measure of interest is what proportion of this population would be deemed to have a result below the lower limit of normal (LLN), which is the 5th centile, suggesting that the result is unusual. The table shows the percentage of each population that falls below this threshold when using Ancestry specific equations on the left and the Global ancestry neutral equations on the right.
| Ancestry Specific | Global | ||||
|---|---|---|---|---|---|
| White | Black | White | Black | ||
| FEV1 | 11.8% | 11.0% | 7.1% | 20.8% | |
| FVC | 6.0% | 7.8% | 2.6% | 15.8% | |
| FEV1/FVC | 13.3% | 10.9% | 15.0% | 10.7% | |
With the ancestry specific equations in the left hand two columns the proportions below the LLN for FEV1 and FVC are similar between Whites and Blacks, but there are slightly more Whites with a low FEV1/FVC. It is expected that about 5% of a completely normal population would have results below the LLN. With obstructive lung conditions being much more prevalent than restrictive the results show an excess of about 6 to 8% with obstructive features and 1 to 2% restrictive.
In the right hand two columns, when using ancestry neutral Global equations, the percentage with FEV1 and FVC < LLN in Whites is almost halved but for Blacks it is almost doubled. The prevalence of airflow obstruction is not particularly changed but severity estimates of obstruction in Blacks will be much worse and a low FVC suggesting restriction much increased. Others have shown this effect with the suggestion of a restrictive defect being twice as prevalent (38% vs 18%) in Blacks [13]. So by ignoring anthropometric differences between peoples of different ancestry one dramatically alters the apparent prevalence of lung function abnormalities.
It has been argued that by using ancestry specific equations this 'normalises' any differences which may be due to remediable causes. However, by confusing anthropometric differences with other remediable causes means the chance of correctly identifying the true causes behind a subject's lower lung function will be lost. Arguments have been raised that by using ancestry neutral equations it is possible to better predict survival from lung function [16]. This line of reasoning implies that the worse mortality for African Americans compared to American Whites should be accounted for by lung function. So, by making lung function appear worse for African Americans, by using ancestry neutral equations, survival differences were better accounted for. This flies in the face of the evidence from the Center for Disease Control and Prevention that the worse mortality in African Americans has nothing to do with respiratory disease or lung function but is due to hypertension, cardiovascular disease, diabetes and gun related deaths [17]. So by ignoring the real differences in the relation between height and lung function for people of different ancestry clinicians are now being falsely led to believe that the worse mortality for African American patients is all due to 'poorer lung function', which allegedly has hitherto been missed by using ancestry specific lung function prediction equations.
So in the face of this sophistry promoting the use of ancestry neutral equations what chance does medical science have of remedying the true causes for worse survival in African Americans and improving their clinical outcomes?
Furthermore, use of ancestry neutral equations, will lead to true disease being missed in non-Hispanic Whites, and for non-Hispanic Blacks the increase in apparent disease will limit work opportunities in certain areas of employment and increase health insurance premiums. These poorer outcomes for people on the basis of their ancestry would constitute racism in medical practice.
Further reading: 18, 19, 20, 21